Targeting resistant germs
Transcribed into the language of chemical formulas, the compounds look as complicated as their name sounds to people not familiar with chemistry. However, this group of substances, called “thienocarbazoles”, can be produced in the laboratory more easily and thus also more cost-effectively. This is an important aspect for a substance that will one day be able to treat bacterial infections even when conventional antibiotics have long since ceased to be effective. Until then, a lot of water is likely to have flowed down the Saale river. “But as of now, the results look very promising,” says Professor Andreas Hilgeroth, who is developing these difficult-to-pronounce substances along with his colleagues at MLU’s Institute of Pharmacy. In doing so, he is tackling a problem that is a burning issue for many doctors.
After all, since World War II, the treatment of bacterial infections has relied on antibiotics, which originally produced moulds, bacteria and other organisms to keep their competitors in check. However, the production of these natural substances and the compounds developed from them is very complex and expensive. Bacteria have long since learned to fend off these antibiotics. Therefore, germs keep popping up which conventional antibiotics are no longer able to combat, especially in hospitals. “This means that we need new active substances to prevent the return of these infectious diseases, an ancient scourge of mankind,” explains Andreas Hilgeroth.
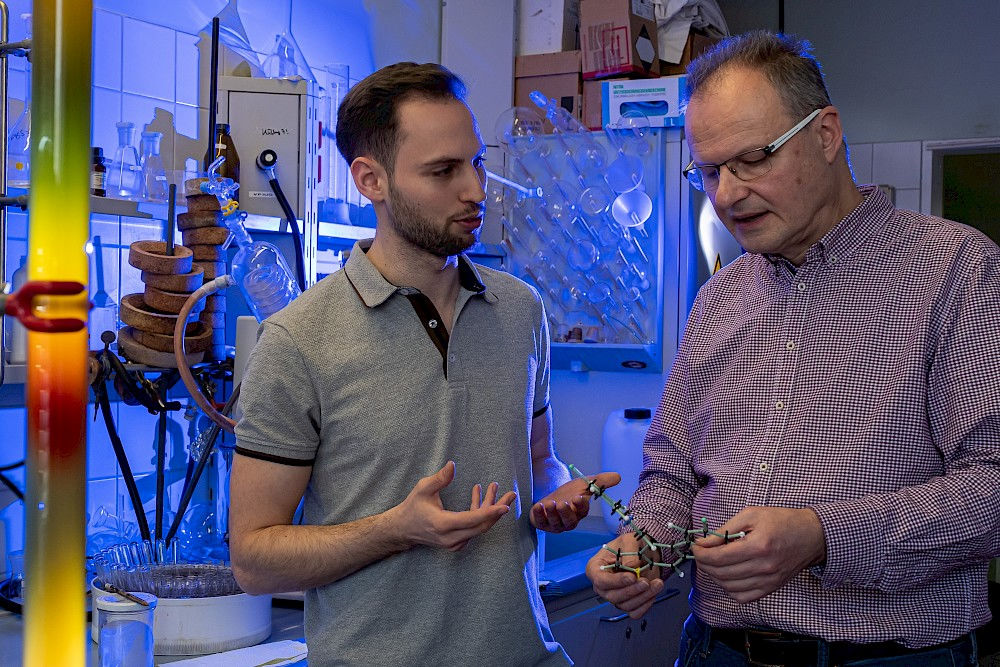
The idea for such a substance was brought to MLU by a young scientist from Egypt. As part of her doctoral thesis, she produced different thienocarbazoles by having relatively simple and well-known chemical compounds react with one another. MLU researcher Marius Seethaler then created several variants of these. This was done without expensive catalysts and high temperatures that require a lot of energy. “In our case, simple and inexpensive acetic acid activates one of the two compounds, which then reacts with the other, ultimately producing the desired substances very easily in a single container,” says Hilgeroth, explaining how the new active substances are produced.
Using Staphylococcus aureus bacteria, MLU researchers Marius Seethaler and Andreas Hilgeroth, together with colleagues from the universities of Würzburg and Greifswald, acted upon their suspicion that these thienocarbazoles might be effective in fighting bacterial infections. Such microorganisms are very widespread and often live on human skin without causing any harm. Only when the immune system is weakened, for example, do the bacteria take advantage of the opportunity to cause an infection. This can lead to skin inflammation, such as boils, as well as inflammation of the lungs or heart, which can sometimes be life-threatening.
Usually such infections can be treated effectively with antibiotics. However, if the germs are already resistant to one or more antibiotic, these weapons against infection prove to be blunt instruments.
Such resistance is particularly common for Staphylococcus aureus. However, Hilgeroth’s new active substances put these bacteria out of action in a completely different way. In some cases they are even more effective than traditional antibiotics, meaning that they should also work against multi-resistant germs. They also help combat Enterococcus faecium. This normally harmless inhabitant of our intestines is not only resistant to various antibiotics, it can also cause infections of the heart, gallbladder and bladder.
“We now have a very clear indication of how our thienocarbazoles work,” reports Hilgeroth. They seem to target an enzyme called “pyruvate kinase”, which plays a crucial role in supplying energy to practically all organisms on earth. However, the thienocarbazoles do not target the active site of the enzyme where the vital reaction of energy metabolism takes place. After all, this area is very similar in different organisms. If a substance takes effect there, it could affect both the dangerous pathogens and the patient in equal measure. However, there are differences near this active site and it is precisely there where the thienocarbazoles attach themselves. It is a site that is typical for a certain group of bacteria including Enterococcus and Staphylococcus bacteria. There, the active substance blocks the active region, switching off both the enzyme and the bacterium without damaging the pyruvate kinases in the animals and humans.
In fact, Hilgeroth and his colleagues have used this targeted substance to eliminate these bacteria in wax moths but not in insects. The MLU researchers therefore have a promising substance at their disposal that might one day be used to combat bacterial infections for which conventional antibiotics are no longer effective.
“Until then, we still have a number of questions that need answering,” says Andreas Hilgeroth. One important question is how the active substances behave inside the organism: Do they reach their target without being degraded first? Might they damage internal organs such as the liver or the heart? Could they alter the genetic make-up, perhaps even cause cancer or impact pregnancy? Even if there is currently no evidence of such problems, answers to several similar questions must be found in meticulously conducted investigations. Then the substances will undergo years of testing on volunteers to check their effects and side effects. Once the thienocarbazoles have surmounted all these obstacles, the first human lives could be saved in about ten years’ time by these substances developed at MLU.
Professor Andreas Hilgeroth
Institute of Pharmacy
Telephone: +49 345 55-25168
Mail: andreas.hilgeroth@pharmazie.uni-halle.de
Further articles
Active ingredient delivery
In order to ensure that medicine only works where it is supposed to, researchers from Halle are investigating new ways to transport active ingredients. Read more
Enzyme adhesive for combating cancer
René Wartner, Andreas Simon and Marcus Böhme have developed a technology that can be used to treat tumours with pinpoint accuracy. Their enzyme adhesive should allow toxins to bind to antibodies and be transported in a targeted way to cancer cells. The three biochemist entrepreneurs plan to market their idea. Read more

