Active ingredient delivery

The single fibres are only about 400 nanometres thick, making them 200 times thinner than a human hair. At the Institute of Pharmacy, doctoral student Benedikt Göttel allows a solution to flow through a needle and then applies an external electrical voltage. “The drop that forms on the needle is stretched into a thin thread by the voltage. Then the thread is dried and collected,” explains Göttel. The method for producing these fibres is called electrospinning, which is widely used by the pharmaceutical industry. Here it will be used to treat eye infections much more effectively than before.
A nonwoven material that looks like a paper tissue slowly forms on the plate below the needle. The solution Göttel is using to spin the fibres contains various polymers and an active ingredient: amphotericin B, which is used to treat fungal diseases in the eye. The advantage of the substance is that it can attack the cell membranes of fungi in a very selective way. And yet, says the pharmacist, amphotericin B is not without its issues. “It does not dissolve well in oil or water.” The active ingredient needs to be combined with excipients in order to dissolve. These excipients include bile salts, which can be problematic in terms of tolerability. During treatment, drops of the drug solution must be administered into the eye once an hour because the eyelid and tear duct transport the drug away too quickly.
“We are working together to try to optimize this,” says Göttel. The nonwoven material, which he is developing in Professor Karsten Mäder’s research group at the Institute of Pharmacy, will be applied to the infected eye during treatment. Göttel has spun the nonwoven from commercially available polymers and has combined the drug with another non-toxic polymer to make it water-soluble. This minimises the harmful side effects on the eye’s cells. The nonwoven is shaped into a contact lens. Once in the eye, the fibres come into contact with tear fluid and form a gel-like substance, which does not disappear so quickly through the tear duct.
Targeted treatment, controlled release, fewer side effects: The pharmaceutical technology group led by Karsten Mäder, who is also the director of the Institute of Pharmacy, specialises in research on this topic. “Some products on the market have less than ideal properties,” he says. His colleagues therefore often work on improving the “packaging” of medically approved active ingredients so that they can be more easily transported inside the human body to the site where they are needed. His team works very closely with physicians from University Hospital Halle, for example from the Oncology Department, Ear-Nose-and-Throat Clinic, the Ophthalmology Department, and the Neurosurgery Department. The placement of the drug carrier directly at the target site, for example in the eye or ear, is one potential option. If the polymers are degradable in the human body, the active ingredients can be released at the target site over days, weeks or months. Another possibility is the production of nanoparticles, which accumulate at the target site and release the active ingredient there in a targeted fashion. Mäder likes to refer to these as active ingredient taxis.
There are many ways to take advantage of improved delivery systems. In addition to polymer contact lenses, Mäder is also developing a nonwoven that can be used following brain surgery. However, the polymers employed in such an application must remain stable for a considerably longer time than those applied to the eyes. They need to be loaded with an active ingredient that protects nerve cells. “At the moment the drug is being injected into the body. However, the dose must be kept low because it can quickly impact the heart,” explains Mäder.
Admittedly, applying drugs locally is not the only way to achieve targeted treatment. “The trend is increasingly moving towards individualised medicine,” says Mäder. Some drugs are only effective if patients have a specific receptor. It is not uncommon for a new drug to be approved before there is evidence for why it works in some people and not in others. According to Mäder, the key question when developing these highly specific active substances is, “What do I want to target, where do I want to change something?” The answer: Just like puzzle pieces that fit together, the molecule of the active ingredient must fit into the structure of the molecule causing the disease - for example an enzyme. But designing a new, perfectly fitting active ingredient is easier said than done. An enormous amount of basic research is required, like that which is being carried out at the University of Halle.
The Institute of Pharmacy in Halle is one of the largest of its kind in Germany. Here, 17 research groups are working on a range of research topics. Some of them are only tasked with studying the appearance of the microscopic structures to which an active substance could dock. Others are designing the corresponding chemical structures on the computer and then checking in the laboratory whether they can be produced at all. Nature is also constantly coming up with new solutions: For example, one research group is investigating traditional African medicinal plants, others are looking for new substances in bacteria. Plants and bacteria often develop very specific defence mechanisms to ward off pathogens and these can also be used in humans.
But no matter how a drug molecule is discovered, Mäder explains, for it to be turned into a targeted drug, its utilisation must be taken into consideration right from the start. The molecules must be able to cope with the chemical conditions inside the body. “In the past, the pharmaceutical industry was mainly focused on maximising effectiveness at the receptor.” But this meant that the highly specific structures could be rendered useless in practice because they were not soluble enough and never reached the target site. “It’s difficult, when the molecule is like a brick,” says the pharmacist.
Today, the development of new drugs places more focus on bioavailability. A biopharmaceutical classification system assigns drugs to four classes depending on how soluble they are and how well they pass through a cell membrane. This is also an important tool for approving so-called generic drugs. Even though they contain the same active ingredient as an original medication, they may contain other excipients. As a specialist in such things, Mäder emphasises that caution must be exercised when assessing the equivalence of generics with the original medication and when comparing generics with each other. After all, excipients not only influence solubility, but also how quickly or how long a drug works. According to the statutory health insurance companies’ so-called aut-idem regulation, pharmacies should dispense an equivalent generic drug made by a low-cost contract manufacturer unless the doctor explicitly prescribes a specific drug. “Several drugs have since been excluded from substitution by the Federal Joint Committee,” says Mäder. The committee, made up of physicians and representatives from health insurance companies and hospitals, decide which medical services are reimbursable by health insurance companies.
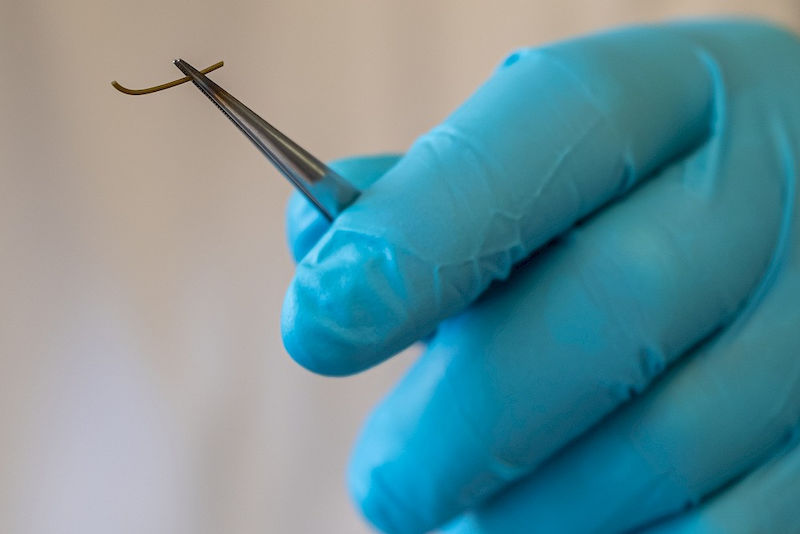
Producing a new drug is complex, stresses Mäder. Development often takes a long time, so that the new drug is only protected against imitation by a patent for a short time. Only one out of thousands of active ingredients produced in laboratories actually reaches the market. Structures produced on the computer often turn out to be impractical. In the case of plant extracts, finding the active molecules or mixtures of molecules among the numerous substances present in the plant and standardising them is often difficult. Many ideas are not pursued because of lack of funding. Millions are spent on preclinical and clinical studies required to approve a drug; it usually takes at least ten years to develop a medicine from an active ingredient. “The worst thing that can happen is for a medicine to succumb at one of the final hurdles,” says Mäder. After all, he says, the goal of the pharmaceutical industry is to make money. This is also why financially unprofitable research, such as the search for new antibiotics, is often only carried out by universities and scientific institutes, mainly using public funds. As part of a DFG-funded research group comprised of scientists from Germany, Israel and Palestine, Mäder’s research group has refined an anti-malarial drug so that it is more absorbable by the body through the intestines, making it very effective. A few months ago, the institute’s director and colleagues filed for a patent for another result of their research: flexible rods made of biodegradable polymers containing an antibiotic. These are used to treat periodontitis by inserting them into the patient’s periodontal pockets. By applying them locally, the undesirable effects of antibiotics on the entire body - such as diarrhoea and skin reactions - can be avoided. Clinical trials are planned in the near future.
The great advantage of the research conducted by Mäders’ group is that it often works with known active ingredients and commercially available excipients. This means that the results can be put to use relatively quickly; it often takes less than ten years for the innovations to be market ready. As a result, the periodontal rods containing the antibiotic complex and the contact lenses with the anti-fungal active ingredient might soon be put to good use in patients.
Professor Karsten Mäder
Institute of Pharmacy
Telephone: +49 345 55-25167
Mail: karsten.maeder@pharmazie.uni-halle.de